Overview of Attention-Deficit/Hyperactivity Disorder (ADHD)
Facts about ADHD:
- ADHD is a neurodevelopmental disorder that includes symptoms of inattention, hyperactivity, and/or impulsivity.
- “ADD” is an old name for the disorder. Asper the current diagnostic manual, the correct name is Attention-Deficit/Hyperactivity Disorder (ADHD). Children can be diagnosed with ADHD inattentive presentation, ADHD hyperactive/impulsive presentation, or ADHD combined presentation (both inattention andhyperactivity/ impulsivity).
- Genetics plays a role: having a parent with ADHD increases the risk of a child developing ADHD.
- Teacher and parent behavior does not cause ADHD, but can have an effect on how often problem behaviors occur and their severity.
- Scientific evidence has disconfirmed that sugar or food dyes cause ADHD.
- There is no evidence that the cycles of the moon or the weather significantly change the behavior of children with ADHD.
- The best way to determine how teacher practices, family events, medication or the environment affect a child’s behavior is to the graph the child’s daily behavior andlook for patterns associated with these events.
- ADHD is a chronic disorder. Just like diabetes, the symptoms and impairments in daily functioning must be managed through intervention over time.
Interventions for ADHD:
1 – on – 1 Counseling
- Although 1-on-1 counseling can be effective for depression and anxiety, it is NOT effective for reducing the symptoms and impairments associated with ADHD. Counselors may be able to teach skills such as social skills or self-regulation strategies to a child with ADHD, however, most children with ADHD will not apply the skills outside of counselling sessions.
Behavioral Intervention
- Research shows that the inattentive and disruptive behaviors associated with ADHD can be significantly reduced with behavioral interventions.
- Behavioral interventions include:
- creating rules, routines, and structure
- teaching rule-following behaviors, self-regulation, and organizational skills
- reinforcing skill development through praise, rewards, and use of appropriate consequences
- Behavioral strategies work best when used consistently.
- Common behavioral interventions include Tier 1 (praise, class rewards) and Tier 2 (Daily Report Card) strategies
Psychostimulant Medication
- Psychostimulant medications such as Adderall, Ritalin, or Concerta, can help reduce the symptoms of ADHD. However, medications are only effective when they are used—that is, if a child stops taking medication, the benefits will cease.
A Closer Look at Tier 2 Behavioral Interventions
Benefits of the Daily Report Card (DRC) over time
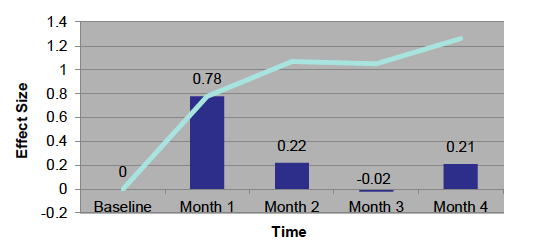
The bar graph in Figure 1 shows that the DRC produces a large benefit in Month 1. The bars for months 2, 3 and 4 indicate that the amount of improvement is less in subsequent months, but improvement does continue. The line on the graph shows that the total amount of improvement continues to increase over the four months. The vertical axis indicates “effect size”. Zero means that there was no change and 1 indicates that the student’s typical days are as good as days that were previously considered his/her best days. One is a large improvement.
An effect size represents the difference between the average behavior during the intervention and the average behavior during baseline.
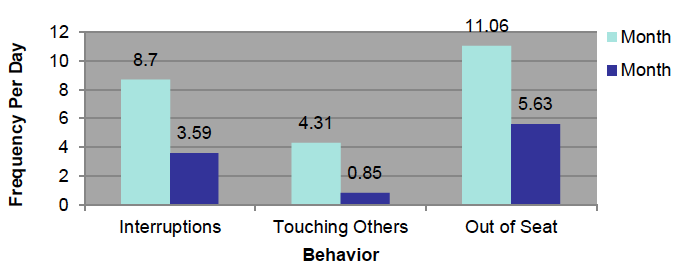
Figure 2 shows that disruptive behaviors can be cut in half over four months of intervention. For example, the frequency of interruptions drops from 8.7 daily to 3.59 daily overtime.
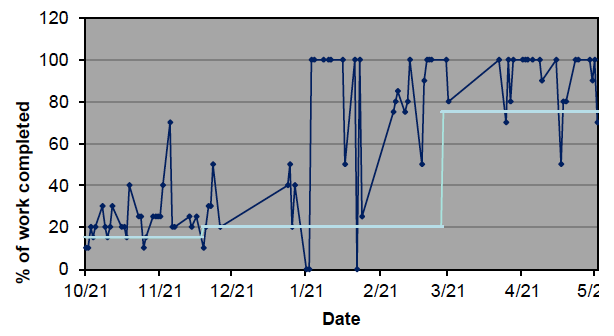
Percentage of Work Completed Per Day
Number of Incidents of Physical Aggression Per Day
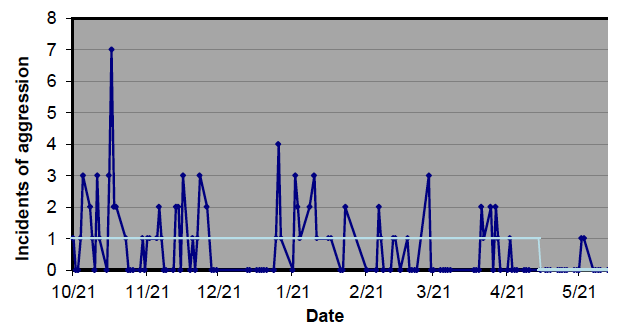
The graphs above show the gains made by a first-grader over the course of a year. Improvement was seen with each month of the intervention. Additionally, work completion remained high (almost 100% of work completed) and aggression was infrequent in the Spring, with continued use of the DRC.
Putting this info to use:
A teacher in your school mentions that they think a child in their classroom has ADHD. You know that this student has previously attended counseling in the community, but the child still appears to be struggling. The teacher is considering asking the parents to place the child on medication because they “don’t know what else to do. Nothing works.”
Based on the information above, what advice would you have for this teacher?